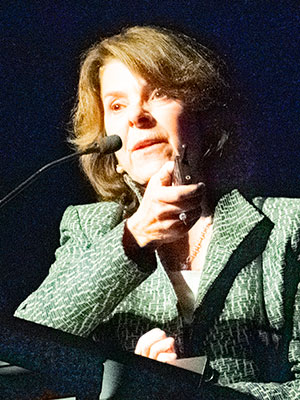
During the annual Oscar S. Gluck, MD Memorial Lecture on Tuesday, Nov. 12, investigator Elizabeth Shane, MD, reviewed the available data and ongoing research on the diagnosis and management of premenopausal osteoporosis.
Dr. Shane, Professor of Medicine at Columbia University Irving Medical Center, New York, said that premenopausal osteoporosis presents a particularly complex clinical challenge because it’s not particularly common and there’s no clear indication for treatment in premenopausal women.
“I think the diagnosis of osteoporosis in premenopausal women is particularly difficult. It’s challenging,” she said. “It’s most secure if you already know that the patient has a secondary cause of osteoporosis that could be affecting their bones, like steroids or rheumatoid arthritis, etc. Or if they’ve had one or more low-trauma fractures.”
Dr. Shane said low bone density as measured by DXA in otherwise healthy women should be interpreted with caution but may reflect low volumetric bone mineral density (BMD) and strength. She also cautioned that bone turnover markers offer limited help in assessing bone turnover in premenopausal women. However, bone biopsies may be helpful if they’re available.
When it comes to managing premenopausal women with osteoporosis, Dr. Shane said the best-case scenario is to find a secondary cause of bone loss and treat that when possible.
“This often gives us the largest improvements in bone density,” she said. “This has been shown with celiac disease, primary hyperparathyroidism, etc. There’s also been some data that show if you control inflammation in inflammatory disease, like RA or inflammatory bowel disease, it can have a beneficial effect on bone density.”
If you can’t find an underlying cause of the bone loss, the dilemma becomes whether to treat.
“Generally, we prescribe conservative measures such as calcium, vitamin D, adequate nutrition, avoiding alcohol and tobacco,” Dr. Shane said. “This is something that will help them from getting worse, but they won’t see significant improvement. Still, most women with low bone density do not require drug therapy, in my view.”
She said she may make exceptions for a patient approaching menopause or who is going through menopause, as women have an increased fracture risk in the first few years after menopause, so clinicians may want to intervene at that point.
However, in an otherwise healthy 30-year-old woman, Dr. Shane said she would follow up with that woman and not treat unless pushed. She reserves drug therapy for women with fractures or declining bone density with conservative treatment or very low BMD.
Finally, Dr. Shane said antiresorptive drugs and teriparatide have been shown to increase BMD in premenopausal women with unexplained bone loss; however, there isn’t data on whether treatment improves fracture risk.
“I don’t think we will ever have that data,” she said. “It’s challenging to get that data in studies of 15,000 postmenopausal women with high rates of fractures. I think the odds we’ll ever have that kind of data in premenopausal women is slim.”
The memorial lecture honors Dr. Gluck’s significant contributions to bone research and is presented each year during the ACR/ARP Annual Meeting by an outstanding investigator in the area of bone and/or bone metabolism research.
